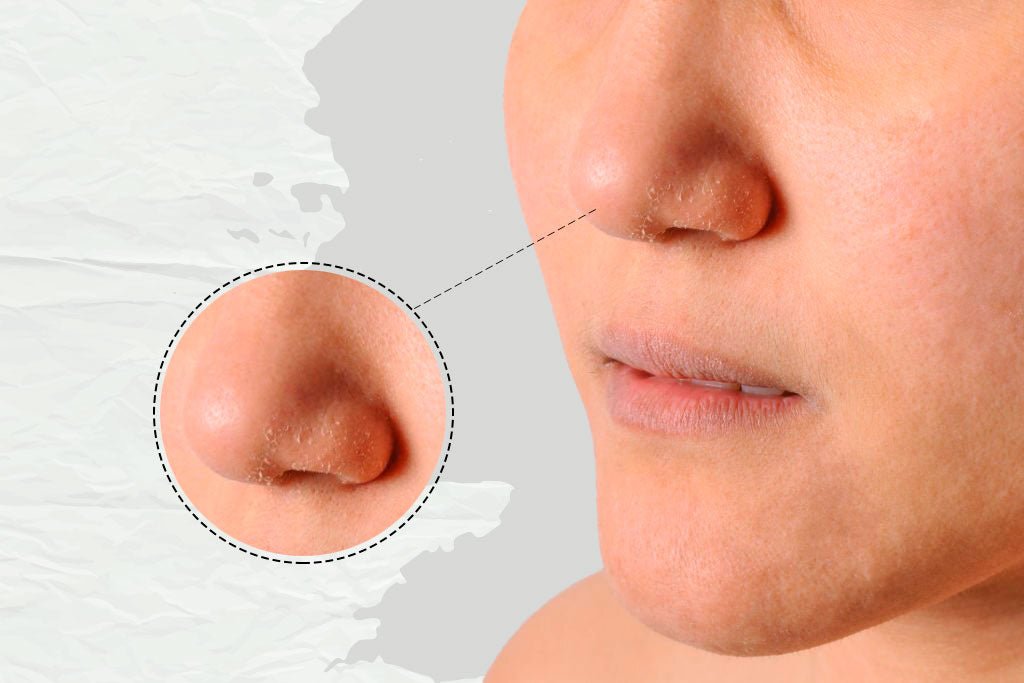
Have you noticed dry white patches on your skin? Don’t worry because you’re not alone, many people experience these dry patches. These dry white patches of skin can feel scaly and rough only in certain areas where it often appears such as face, eyelids, elbows, lower arms, hands or wrists, feet or ankles etc. Let’s understand what this dry white parches are and what they mean.
In This Article
What are dry white patches found on the face and skin?
Dry white patches on the face and skin can be caused by a variety of factors, including dry skin, eczema, and dermatitis. These conditions can cause the skin to become dry and flaky, leading to the development of white patches.
If you are experiencing dry white patches on your face and skin, it is important to consult a dermatologist or other healthcare provider to determine the cause and receive appropriate treatment.
Causes of dry white patches on the face
There are several potential causes of dry white patches on the face, including:
- Dry skin: Dry skin is a common cause of dry white patches on the face. Dry skin can be caused by a variety of factors, including cold weather, hot showers, and dry air.
- Eczema: Eczema is a type of skin irritation that can cause dry, red, and itchy patches to develop on the skin.
- Dermatitis: Dermatitis is a general term used to describe skin irritation and inflammation. There are several different types of dermatitis, including contact dermatitis, which occurs when the skin comes into contact with an irritant, and atopic dermatitis, which is a type of eczema.
- Other skin conditions: Dry white patches on the face can also be caused by other skin conditions, such as psoriasis or fungal infections.
1. Causes of dry white patches on the face due to vitamin deficiency
Certain vitamin deficiencies can lead to the development of dry white patches on the skin, although this is not a common cause. Some vitamins that play a role in healthy skin include:
- Vitamin A: A deficiency in vitamin A can lead to dry, flaky skin and a loss of elasticity.
- Vitamin B: B-vitamin deficiencies, including deficiencies in B1 (thiamin), B2 (riboflavin), and B3 (niacin), can cause skin problems, including dry skin on face.
- Vitamin C: Vitamin C is important for the production of collagen, a protein that helps to keep skin firm and healthy. A deficiency in vitamin C can lead to dry, rough skin and a slower healing time for cuts and wounds.
- Vitamin D: Vitamin D is important for the health of the skin and a deficiency in this vitamin can lead to dry, flaky skin.
If you are experiencing dry white patches on your face and are concerned about a possible vitamin deficiency, it is important to consult a healthcare provider for a proper diagnosis and treatment. The provider will consider your medical history and may recommend blood tests to check for vitamin deficiencies. Treatment may include taking vitamin supplements and making changes to your diet to increase your intake of certain vitamins.
2. Causes of dry white patches on the face during pregnancy
There are several potential causes of dry white patches on the face during pregnancy, including:
- Hormonal changes: Pregnancy is associated with hormonal changes that can affect the skin. These changes can lead to dryness, flakiness, and the development of white patches on the skin.
- Dehydration: Pregnancy can increase the risk of dehydration, which can cause the skin to become dry and flaky.
- Dry skin: Pregnancy can also cause dry skin, which can lead to the development of dry white patches.
- Other skin conditions: Pregnancy can exacerbate certain skin conditions, such as eczema and dermatitis, which can cause dry white patches to develop on the skin.
If you are pregnant and experiencing dry white patches on your face, it is important to consult a healthcare provider for a proper diagnosis and treatment. The provider will consider your medical history and may recommend certain skincare products or medications to help manage the dryness and flakiness.
Causes of dry white patches on the face during winter
There are several potential causes of dry white patches on the face during the winter months, including:
- Dry air: The cold, dry air of winter can cause the skin to become dry and flaky, leading to the development of dry white patches.
- Hot showers: Taking hot showers or baths can strip the skin of its natural oils, leading to dryness and flakiness.
- Cold weather: Exposure to cold weather can cause the skin to lose moisture, leading to dryness and the development of white patches.
- Heating: Indoor heating can also contribute to dryness of the skin by reducing the humidity in the air.
To help prevent dry white patches on the face during the winter, it is important to keep the skin moisturised and to use lukewarm water instead of hot water when showering or bathing. It is also helpful to use a humidifier to increase the humidity in the air and to limit exposure to cold, dry air. If you are experiencing dry white patches on your face and are concerned about the cause, it is important to consult a healthcare provider for a proper diagnosis and treatment.
Dry white patches in children and adults
A. In Children
Dry white patches on the skin can occur in children and adults. In children, these patches may be caused by the same factors that cause dry white patches in adults, such as dry skin, eczema, and dermatitis. In addition, children may be more prone to developing dry white patches due to their more sensitive skin.
If your child is experiencing dry white patches on their skin, it is important to consult a healthcare provider for a proper diagnosis and treatment. The provider will consider your child's medical history and may perform a physical examination and possibly a skin biopsy to determine the cause of the dry white patches. Treatment may include the use of moisturizers, corticosteroid creams, and other medications, depending on the underlying cause of the patches.
B. In Adults
In adults, these patches may be caused by dry skin, eczema, dermatitis, or other skin conditions. Dry skin can be caused by a variety of factors, including cold weather, hot showers, dry air and nutritional deficiencies.
If you are an adult experiencing dry white patches on your skin, it is important to consult a healthcare provider for a proper diagnosis and treatment. The provider will consider your medical history and may perform a physical examination and possibly a skin biopsy to determine the cause of the dry white patches. Treatment may include the use of moisturizers, corticosteroid creams, and other medications, depending on the underlying cause of the patches.
What are itchy white patches on the face?
Itchy white patches on the face can be caused by a variety of factors, including dry skin, eczema, and dermatitis. These conditions can cause the skin to become dry, red, and itchy, leading to the development of white patches.
In some cases, itchy white patches on the face may be a sign of a more serious condition, such as a fungal infection or an allergic reaction.
What are fungus white spots on the face?
Fungus white spots on the face are a type of fungal infection known as tinea versicolor. Tinea versicolor is caused by a type of yeast that is naturally present on the skin. When the yeast grows out of control, it can cause a rash with white or light-colored patches to develop on the skin. Tinea versicolor is most commonly found on the chest, back, and upper arms, but it can also affect the face.
Tinea versicolor is typically treated with antifungal medications, which can be applied topically or taken orally. If you are experiencing fungus white spots on your face and are concerned about the cause, it is important to consult a healthcare provider for a proper diagnosis and treatment. The provider will consider your medical history and may perform a skin scraping or culture to confirm the diagnosis of tinea versicolor.
Common Myths & Facts related to Dry White Patches on Skin
Myth 1: Dry white patches on the face are always a sign of poor hygiene.
Fact: Dry white patches on the face can result from various factors, including skin conditions like eczema, psoriasis, or fungal infections, which have nothing to do with poor hygiene.
Myth 2: Only people with dry skin get dry white patches.
Fact: White patches can affect anyone, regardless of their skin type. They can be caused by a range of factors including vitamin deficiencies, fungal infections, or skin conditions like vitiligo.
Myth 3: White dry patches will go away on their own if ignored.
Fact: While some dry white patches may fade over time, others require treatment. Ignoring persistent patches can lead to worsening conditions or underlying health issues being overlooked.
Myth 4: Dry White patches are always a sign of a serious medical condition.
Fact: While some white dry patches may indicate an underlying condition, many are benign and caused by factors like dry skin or minor infections. A dermatologist can help determine the cause.
Myth 5: Sun exposure will help treat white dry patches on the face.
Fact: Sun exposure can worsen certain conditions like vitiligo or make white dry patches on the face more noticeable. It's important to protect your skin with gel based sunscreen and seek appropriate treatment.
Myth 6: All white patches are caused by fungal infections.
Fact: While fungal infections like tinea versicolor can cause white patches, other conditions such as eczema, psoriasis, or ichthyosis vulgaris can also be culprits.
Myth 7: You can scrub white dry patches on your face away.
Fact: Scrubbing dry white patches can irritate the skin and make the condition worse. Gentle care and appropriate treatment are needed to address the underlying cause.
Myth 8: Home remedies can cure all white patches.
Fact: While some home remedies may provide temporary relief, professional diagnosis and treatment are often necessary for persistent or severe dry white patches.
Myth 9: White patches mean your skin is permanently damaged.
Fact: Many causes of white patches, like dry skin or mild fungal infections, are treatable and reversible with proper care and treatment. Permanent damage is rare.
Myth 10: White patches are contagious.
Fact: Most white patches are not contagious. Conditions like eczema, vitiligo, or psoriasis are not spread from person to person, although some fungal infections may be mildly contagious.
What are the treatment options to remove dry white patches?
The treatment options for removing dry white patches on the skin will depend on the underlying cause of the patches. Some potential treatment options may include:
- Moisturisers: Moisturizers can help to replenish lost moisture and prevent further dryness of the skin.
- Corticosteroid creams: Corticosteroid creams can help to reduce inflammation and itchiness associated with certain skin conditions, such as eczema and dermatitis.
- Antifungal medications: If the dry white patches are caused by a fungal infection, such as tinea versicolor, antifungal medications may be prescribed to treat the infection.
- Other medications: Depending on the underlying cause of the dry white patches, your healthcare provider may prescribe other medications to help manage the condition.
It is important to follow the treatment plan recommended by your healthcare provider in order to effectively manage the dry white patches and improve the appearance of your skin. In addition, it is important to practice good skincare habits, such as using a gentle cleanser, avoiding hot water and harsh soaps, and applying a moisturizer regularly to help prevent the dry white patches from returning.
Home remedies to remove dry white patches?
There are several home remedies that may help to remove dry white patches on the skin and improve the overall appearance of the skin. Some potential options include:
- Moisturise regularly: Applying a moisturizer to the skin on a regular basis can help to keep the skin hydrated and prevent dryness.
- Use gentle cleansers: Avoiding harsh soaps and using non-drying gentle face wash cleansers can help to prevent further dryness of the skin.
- Avoid hot water: Taking lukewarm showers or baths instead of hot water can help to prevent the skin from becoming dry and flaky.
- Use a humidifier: Using a humidifier to increase the humidity in the air can help to keep the skin moisturized and prevent dryness.
- Avoid irritants: Avoiding irritants, such as certain soaps, perfumes, and harsh chemicals, can help to prevent the development of dry white patches on the skin.
- Protect the skin from the sun: Using sunscreen with a high SPF and wearing protective clothing can help to prevent sun damage, which can contribute to dryness of the skin..
Conclusion
While there are multiple reasons for you to possibly develop dry white patches on your skin, it is important to know that you must immediately consult with your dermatologist or your healthcare provider for the right diagnosis and treatment plan. It is also important to be consistent with your treatments, in order to improve the condition of your skin and keep it healthy and glowing.
FAQ's
What are the potential long-term effects of having white spots on the skin, even if they are currently benign?
White spots on the skin may not be harmful now, but they can have long-term effects. These spots can be a sign of deeper health conditions. Vitiligo, for example, is a skin problem where cells that make skin color are lost. This can lead to white spots. Vitiligo isn't dangerous, but it can increase the risk of sunburn and skin cancer because the affected skin has less protection. It can also lead to social issues like stigma and discrimination, which can hurt mental health. White spots can also be linked to autoimmune diseases. If these diseases are not treated, they can pose serious health risks. It's crucial to get an early diagnosis and proper treatment for white spots to prevent potential long-term problems.
Are there any lifestyle changes or preventative measures that can be taken to reduce the risk of developing white spots on the skin?
Preventing white spots on the skin involves sun protection, avoiding tanning beds, staying hydrated, eating a balanced diet, managing stress, treating skin conditions promptly, conducting regular skin checks, and refraining from scratching or picking at the skin. These measures collectively reduce the risk of white spot formation and promote skin health. Consulting a dermatologist for personalized advice is recommended for any concerning changes in the skin.
Are there any home remedies or lifestyle changes that can help manage white spots?
When dealing with white spots on the skin caused by various factors, there are effective home methods and lifestyle choices you can adopt. It's important to prioritize keeping the affected area well-moisturised, avoiding excessive sun exposure, and considering dietary adjustments to support skin health. Additionally, topical remedies such as aloe vera or tea tree oil can be beneficial, along with managing stress effectively and maintaining good hygiene practices. While these steps can provide some relief, it's essential to consult a healthcare professional for an accurate diagnosis and personalized advice. SkinQ offers targeted solutions that also help curb dark spots, including moisturizing creams, broad-spectrum gel sunscreens, and advanced formulations enriched with brightening ingredients like vitamin C.
If I have white spots, what is the best way to get a diagnosis?
For white spots on your skin, consult a dermatologist for an accurate diagnosis. They are medical experts trained in skin issues. During your appointment, they will inspect the spots, ask about your medical history, and potentially perform tests to determine the cause. Avoid self-diagnosis as similar-looking skin conditions have different underlying issues. Professional medical guidance is vital for a precise diagnosis and suitable treatment.